|
CASE REPORT |
https://doi.org/10.5005/jp-journals-10033-1512
|
Type VI Choledochal Cyst: A Rare Case Presenting with Acute Pancreatitis
1–4Department of General Surgery, Postgraduate Institute of Medical Education and Research, Chandigarh, India
Corresponding Author: Kailash Chand Kurdia, Department of General Surgery, Postgraduate Institute of Medical Education and Research, Chandigarh, India, Phone: +91 6394358323, e-mail: drkurdia@gmail.com
How to cite this article: Agarwal A, Jayant D, Kurdia KC, et al. Type VI Choledochal Cyst: A Rare Case Presenting with Acute Pancreatitis. World J Lap Surg 2022;15(3):255–257.
Source of support: Nil
Conflict of interest: None
Received on: 29 June 2021; Accepted on: 06 September 2022; Published on: 07 December 2022
ABSTRACT
Choledochal cyst (CDC) of cystic duct, i.e., choledochal cyst type VI is an extremely rare clinical entity, with few case reports only. Even the Todani classification of choledochal cyst does not include as a separate entity. Most of choledochal cyst VI is asymptomatic. For an accurate diagnosis, magnetic resonance cholangiopancreatography (MRCP) is required. There is no consensus regarding the management of the cystic duct cyst due to the rarity of the disease, but treatment alternatives extend from laparoscopic cholecystectomy to complete excision of the biliary duct with bilio-enteric reconstruction. We present a case of middle-aged woman who presented with biliary pancreatitis and managed with interval laparoscopic cholecystectomy. Choledochal cyst type VI had been identified intraoperatively.
Keywords: Acute pancreatitis, Intraoperative diagnosis, Type VI choledochal cyst.
BACKGROUND
Choledochal cysts are focal or diffuse dilatations of a biliary tree that are believed to be congenital. They may occur as single or multiple cysts involving an extrahepatic or intrahepatic biliary tree. The incidence of 1 in 1000 persons is seen in Asia, with higher rates seen in Japan.1 Cystic malformations of cystic ducts i.e. CDC type VI are uncommon with few cases reported in the literature. These are often misdiagnosed or undiagnosed preoperatively. Preoperative diagnosis and appropriate management require awareness of CDC type VI. In this case report, we report an instance of a 45-year-old lady presenting with acute gallstone-induced pancreatitis managed conservatively. No cystic malformation was identified preoperatively but the cystic duct cyst was identified intraoperatively and managed with laparoscopic cholecystectomy.
CASE DESCRIPTION
A 45-year-old lady presented to the emergency department with acute onset severe pain abdomen in the epigastric region, radiating to back for the last 5 days, associated with recurrent bilious vomiting. No history of jaundice, fever, obstipation, and abdomen distension. On assessment, the patient had a pulse rate of 100 per minute, BP of 130/80 mm of Hg, respiratory rate of 20 per minute, and afebrile. Per-abdominal examination, the patient had tenderness in the epigastric region.
INVESTIGATION
Blood workup showed an elevated serum amylase level of 1265 U/L. Ultrasound of the abdomen reported cholelithiasis with multiple calculi and choledocholithiasis, but the pancreas appears normal. Contrast-enhanced CT reported grossly distended gallbladder with multiple calculi and no wall edema. Common bile duct (CBD) dilated, with a diameter of 14 mm and multiple stones in the lumen.
TREATMENT
She underwent ERCP and CBD clearance and stenting. The patient was treated with IV fluid and analgesics. After satisfactory clinical improvement, the patient was discharged.
Four weeks later, she underwent laparoscopic cholecystectomy. On laparoscopy, the gallbladder was distended and mildly inflamed, Calot’s triangle dissected, and critical view of safety was demonstrated. After dissection, we found that there was focal dilatation around a 10-mm cystic duct present, and proximal and distal to dilation, there was waisting present (Fig. 1). The cystic duct was completely dissected till junction to the common hepatic duct (CHD). Laparoscopic cholecystectomy was completed with an application of hemolock clip just adjacent to the junction of the cystic duct and CHD. On the cut section of the specimen, there was no evidence of any mucosal irregularities in the gall bladder and CDC.
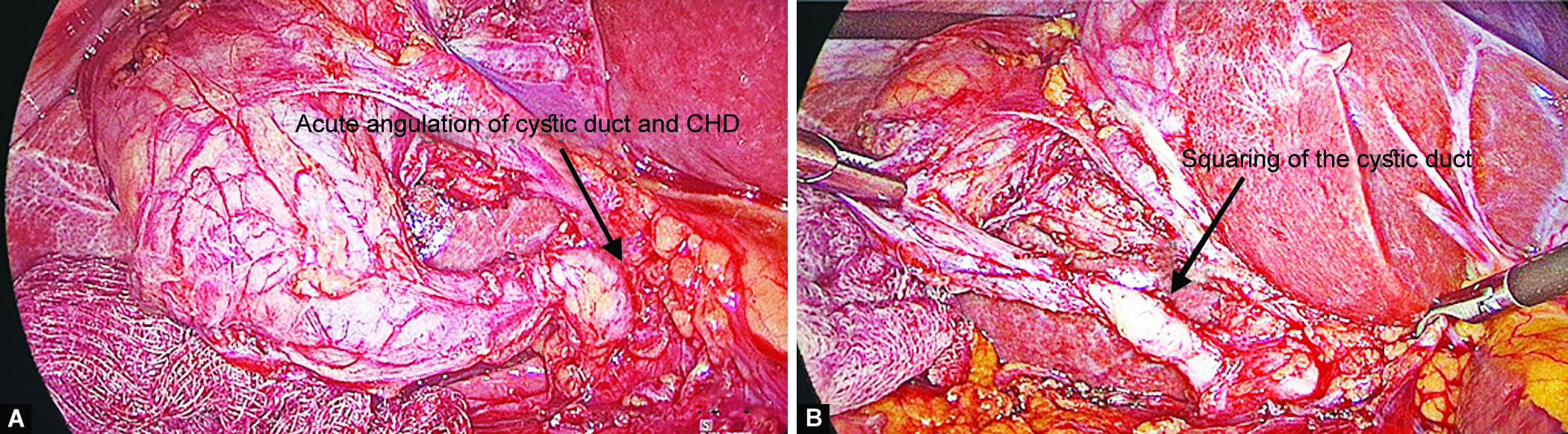
Figs 1A and B: Laparoscopy showing choledochal cyst of the cystic duct with a narrow outlet of the cystic duct into CHD. (A) An acute angulation of the cystic duct with CHD; (B) The squaring of the cystic duct
OUTCOME AND FOLLOW-UP
The postoperative course was uneventful. Magnetic resonance cholangiopancreatography done after 9 months of surgery showed no extrahepatic biliary cystic dilation. It showed normal intrahepatic and extrahepatic biliary systems (Fig. 2).

Fig. 2: Postoperative MRCP showing normal biliary system
DISCUSSION
Choledochal cyst is traditionally classified by Alonso-Lej and associates, which was later modified by Todani and colleagues in 1977 into five types to include intrahepatic cystic dilatation.1 Choledochal cyst type VI was first identified by Bode and Aust in 1983, where the patient presents with acute cholangitis.2 It was Serradel et al. in 1991, who recommended the incorporation of cystic dilation of the cystic duct as a CDC type VI in the Todani classification.3 In the review of literature, there are less than 50 cases reported to date. In most of the case reports, the cystic duct cyst presented as cholelithiasis and was identified intraoperatively.
A patient with a CDC VI can present to the hospital at any age. However, no sex predilection for cystic duct cyst was found in the literature of 10 cases over a period of 2 years, as reported by Maheshwari in 2012.4
Most of these were detected intraoperatively or occasionally on imaging for evaluation of biliary symptoms mostly epigastric and/or right hypochondrium pain. It is also reported as associated with complicated biliary disease, e.g., common hepatic duct obstruction due to the mass effect of cyst or inflammation from cholangitis, biliary pancreatitis, and rarely reported biliary cancer.4–6
Choledochal cyst is an established risk factor of biliary cancer and reported incidence varies and depend at age of diagnosis, the incidence of cancer is 0.7% in the patient under 10 years of age, 6–8% in the patient’s second decade, and 14.3% after 20 years of age and as high as up to 50%.7 Choledochal cyst, though rarely, is also associated with carcinoma gall bladder, periampullary carcinoma, and pancreatic carcinoma. These carcinomas should be excluded before attempting any surgical procedure. The basic principle of surgery of nonmalignant choledochal cyst requires complete excision of the cystic wall.
The diagnosis of CDC type VI requires high suspicion. Abdominal ultrasound is a good initial screening tool to identify any cystic lesion. The abnormality of the cystic duct can be localized with ultrasound by tracing its connection to the gallbladder. However, an operator-dependent property of ultrasound may fail to delineate the biliary origin of the cyst. The normal diameter of the cystic duct varies from 1 to 5 mm. A CDC of the cystic duct is defined as the diameter of the cystic duct of more than 5 mm without any evidence of biliary obstruction. Any nonvascular dilated cystic structure near the porta hepatis should be evaluated for its relationship with the CBD, cystic duct, and gallbladder and its connection with the biliary tract.4
CT scan helps in accessing hepatobiliary and pancreatic anatomy and evaluation of possible malignancy but failed to show pancreaticobiliary maljunction. Magnetic resonance cholangiopancreatography appears superior to CT scan for defining pancreaticobiliary maljunction. The gold standard investigation for the diagnosis of choledochal cyst is cholangiography. Cholangiography is effective in demonstrating the anatomy of the biliary tree, stone, obstruction, and pancreaticobiliary maljunction. The only disadvantage of cholangiography is that it is an invasive method.7
Typical radiological features of CDC type VI are acute angulation of cystic duct and common hepatic duct junction with a distinct plane, squaring and dilatation of the cystic duct, a normal or wide outlet of the cystic duct into CHD, and associated pancreaticobiliary maljunction.4 In our patient intraoperative findings showed acute angulation of cystic duct and common hepatic duct junction with a distinct plane, squaring, and dilatation of the cystic duct, which were similar to radiological findings and confirmed the diagnosis of type VI CDC.
Treatment of cystic duct cyst includes complete excision of cystic duct cyst with cholecystectomy. For the cystic duct cyst with a narrow outlet of the cystic duct into the common hepatic duct, complete excision of the cystic duct cyst with cholecystectomy can suffice. It can be accomplished laparoscopically by clipping the cyst just adjacent to the opening in the CHD, as done in our case. Due to the presence of anatomical difficulty and associated biliary anomalies, which are seen in most reported cases in the literature, laparoscopic cholecystectomy can be done with a low threshold for conversion to open cholecystectomy.5
Cyst with the wide outlet of the cystic duct into the common hepatic duct, open cholecystectomy with excision of cystic duct cyst up to CHD and CBD with bilioenteric reconstruction, to remove the entire cystic epithelium. For bilioenteric reconstruction, Roux-en-Y hepaticojejunostomy is recommended. Although another method of bilioenteric reconstruction like choledochoduodenostomy can be performed.5
CLINICAL SIGNIFICANCE
With advancements made at diagnostic tools and a better understanding of this type of pathology, more cystic lesions of cystic duct can be identified preoperatively. Preoperative diagnosis can help in better management of the patient.
ORCID
Ambuj Agarwal https://orcid.org/0000-0002-5692-892X
Divij Jayant https://orcid.org/0000-0002-1839-228X
Kailash Chand Kurdia https://orcid.org/0000-0002-9600-7981
Arunanshu Behera https://orcid.org/0000-0003-0954-0372
REFERENCES
1. Todani T, Watanabe Y, Narusue M, et al. Congenital bile duct cysts: classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg 1977;134(2):263–269. DOI: 10.1016/0002-9610(77)90359-2.
2. Bode WE, Aust JB. Isolated cystic dilatation of the cystic duct. Am J Surg 1983;145(6):828–829. DOI: 10.1016/0002-9610(83)90152-6.
3. Serradel AFS, Linares ES, Goepfert RH. Cystic dilatation of the cystic duct: a new type of biliary cyst. Surgery 1991;109(3 Pt 1):320–322. PMID: 2000564.
4. Maheshwari P. Cystic malformation of cystic duct: 10 cases and review of literature. World J Radiol 2012;4(9):413–417. DOI: 10.4329/wjr.v4.i9.413.
5. Amarjyothi JMV, Ramasamy V, Jesudasan J, et al. Type VI choledochal cyst – case report and review of literature. Surg J (N Y) 2019;5(3):e82–e86. DOI: 10.1055/s-0039-1693652.
6. Reddych VV, Kumar A, Aggarwal M, et al. Type VI choledochal cyst with carcinoma gall bladder. BMJ Case Rep 2019;12(12):e232715. DOI: 10.1136/bcr-2019-232715.
7. Melton GB, Lillemoe KD. Choledochal cyst and biliary stricture. In: Zinner MJ, Ashley SM, editors. Maingot’s Abdominal Operations, 11th ed. United States of America: Mc Graw Hill, 1997:889–920.
________________________
© The Author(s). 2022 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.