|
CLINICAL TECHNIQUE |
https://doi.org/10.5005/jp-journals-10033-1518
|
Scarless Appendectomy in Children. Is it Safe? Our Initial Single-center Experience
1University of Strasbourg, Strasbourg, Alsace, France; Hopitaux Civils De Colmar, Colmar, Haut-Rhin, France
2Department of Medical Biology, Saint Joseph Hospital, Paris, France
3Department of Public Health, Colmar Civilian Hospital, Colmar, Alsace, France
4Department of Pediatric Surgery, Colmar Civilian Hospital, Colmar, Alsace, France
Corresponding Author: Sandy F Jochault-Ritz, Department of Pediatric Surgery, Colmar Civilian Hospital, Colmar, Alsace, France, Phone: +0033682041857, e-mail: sandy.jochault-ritz@ch-colmar.fr
How to cite this article: Akkary R, Doumat JG, Jochault LH, et al. Scarless Appendectomy in Children. Is it Safe? Our Initial Single-center Experience. World J Lap Surg 2022;15(3):272–275.
Source of support: Nil
Conflict of interest: None
Received on: 04 May 2021; Accepted on: 06 September 2022; Published on: 07 December 2022
ABSTRACT
Purpose: Since the description of laparoscopic appendectomy, the surgeons are trying to develop techniques using less incisions. We describe our initial experience with the transumbilical laparoscopic-assisted appendectomy (TULAA) in children.
Materials and methods: A prospective, single surgeon, single-center study was conducted. The technique was described (Video). The rates of conversion of intraoperative complications and of postoperative complications were noted. Risk factors for conversion were analyzed.
Results: Forty patients were included. Conversion to a classical 3-port technique was done in 13 cases. The only intraoperative complication was an epiploic bleeding encountered in 1 patient. The only postoperative complication was an umbilical abscess in 2 patients. A scarless abdomen was noted 1 month postoperatively.
Conclusion: Transumbilical laparoscopic-assisted appendectomy had combined the exposure advantages of laparoscopy and the low cost of open surgery. Despite the small population number, it seems to be safe, reproducible, and effective, and it had superior esthetic advantages.
Clinical significance: Trans-umbilical laparoscopic-assisted appendectomy reduces the incisions needed to do an appendectomy with no increased risk in complications when compared to the traditional techniques.
Keywords: Appendectomy, Laparoscopy, Single trocar surgery.
INTRODUCTION
Open appendectomy, first described in the 19th century,1 remained the treatment of choice of appendicitis till the introduction of laparoscopic appendectomy.2 Many innovative minimal invasive techniques have been developed,3,4 trying to decrease the number of ports used in the classical 3-port laparoscopic technique. The trans-umbilical single incision laparoscopic appendectomy uses the minimum of laparoscopic instruments for the exposure, and appendectomy is done extracorporeally like in the open technique.5,6 Transumbilical laparoscopic-assisted appendectomy thus combines the advantageous exposure of laparoscopy and the low cost of open surgery.7 Once a new surgical technique is adopted, assuring the safety of the technique during the learning phase might be challenging.8 In this paper, we described the initial experience of one surgeon started adopting the TULAA. The aim was to highlight a simple and reproducible technique, that was forgotten. We described the technique, its advantages, and its limitations. We analyzed the children operated using this technique and their complications.
MATERIALS AND METHODS
All pediatric patients (age ≤18 years) operated for appendicitis by a single surgeon in a single center between November 2018 and October 2019 were prospectively studied. Upon patient presentation, all patients had a basic blood work out and abdominal echography. CT scanner was not done. Patients with a preoperative suspicion of generalized peritonitis on the initial evaluation were directly operated by a classic 3-port approach, so TULAA was not attempted, and hence they were excluded. All patients with appendicular phlegmon or abscess on the initial evaluation were treated medically. After a 10 weeks interval, they were operated according to TULAA. All other patients were operated according to TULAA. Only patients operated primarily according to TULLA were included. The operative time (OT) was noted. The rate of conversion was calculated. Conversion was either to the classical 3-port approach or to laparotomy. Risk factors for conversion were identified. Intraoperative complications like intestinal perforation and bleeding were reported. Length of stay (LOS) was studied. Patients were followed till March 2021. Follow-up was done clinically. Postoperative complications, like intra-abdominal abscess, skin infection, intestinal obstruction, and incisional hernia were reported. All parents were educated about the small but still existing risk of intestinal obstruction.
The technique of TULAA (Video 1).
All patients were asked to empty their bladders before the surgery. Patients were positioned supine with the left arm tucked. All surgeries were done under general anesthesia. After vigorously cleansing the umbilicus, the umbilicus was pulled out using two Allis forceps. A vertical trans-umbilical incision was made. Subcutaneous fat and fascia were cut to allow entry and direct vision into the peritoneal cavity. A sufficient incision allowed the introduction of the surgeon’s little finger. A single 10 mm umbilical port was introduced. A 10 mm 0-degree operative telescope with a 6 mm working channel was used (Fig. 1). Patients were positioned in a Trendelenburg position with the table tilted toward the patient’s left side. A tracheal aspiration tube connected to a feeding syringe was inserted in the working channel and used in order to aspirate the intra-abdominal liquid. A grasper was used in order to bluntly liberate the appendix and the cecum. The peritoneal attachments of the cecum and the appendix were bluntly divided. When those attachments were judged thick, they were coagulated using a monopolar power source connected to the grasper. Minimal liberation was needed. The extent of liberation was judged sufficient when, despite the presence of the pneumoperitoneum, the appendix’s tip reached the umbilical port. The appendix was trapped by its tip and exteriorized along with the cecum through the umbilical incision after clearing the pneumoperitoneum. An extracare must be practiced while exteriorizing a perforated or gangrenous appendix. At skin level, the mesoappendix was ligated using a 3-0 multi-filament braided woven absorbable suture. The base was ligated using a 0 multi-filament braided woven absorbable suture. Extracorporeal appendectomy was done (Fig. 2). The stump was then coagulated. Vigorous incisional cleansing was always done before the closure. During every exploration according to TULAA, the operating room was prepared for a possible conversion to 3-port classical technique.
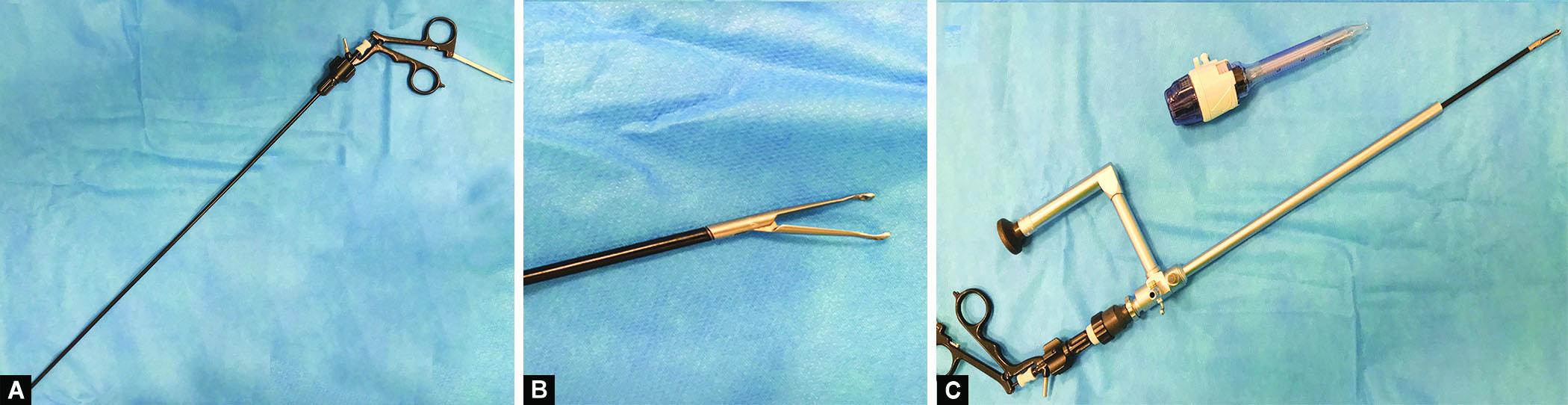
Figs 1A to C: All the needed instruments. (A) The grasper; (B) The tip of the grasper; and (C) The grasper in the telescope with the 10 mm port
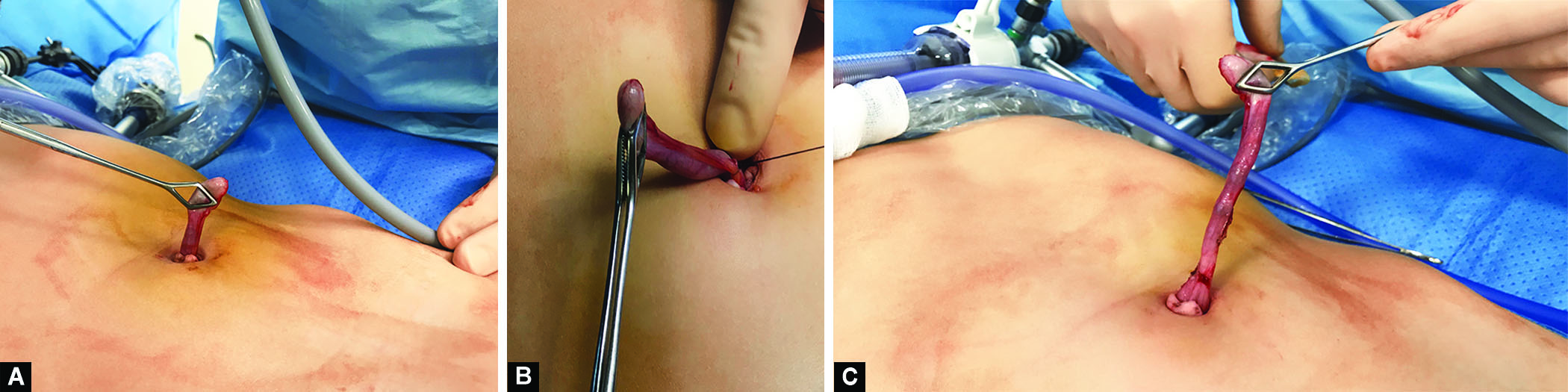
Figs 2A to C: Extracorporeal steps. (A) Exteriorization of the appendix; (B) Ligation of the mesoappendix; (C) The cecum and the base of the appendix had reached skin level
RESULTS
Fifty-five patients were operated for appendicitis. Fifteen patients operated directly according the classical 3-port technique. Forty patients were initially operated according to TULAA. Median follow-up was 22 (17–27) months. Twenty-five patients were males (male to female ratio: 1.7). The mean age was 10 (3.9–17) years. The mean weight was 37 (9–115) kg. The mean duration of evolution before the presentation to emergency room was 43 (8–120) hours. Mean CRP was 58 (1–107) mg/L. Mean leukocytes count was measured at 15 (6–30) giga/L. Mean polynuclear neutrophils count was 11.8 (1.3–27) giga/L. On preoperative ultrasonography, intra-abdominal effusion was seen in 10 patients and appendicolith was seen in 10 patients. Intraoperative diagnosis was early appendicitis in 12 patients, preperforative appendicitis in 14 patients, localized peritonitis in 10 patients, and generalized peritonitis in 2 patients. Two patients had interval appendectomy according to TULAA. Conversion to a 3-port traditional technique was done in 13 patients. The diagnosis in those was, early appendicitis in 6 patients, preperforative appendicitis in 5 patients, and generalized peritonitis in the remaining 2 patients. The conversion was due to a retrocecal or a subserosal appendicitis with or without a non-mobile-fixed cecum in 7 patients. In 2 patients, it was due to generalized peritonitis. In 1 patient, it was due to short appendiceal vessels. In 1 patient, it was related to retroileal appendicitis. In 1 patient, it was secondary to morbid obesity and hence difficulty of extracorporeal ligation of the appendiceal vessels. In 1 patient, it was due to accidental epiploic bleeding. No conversion to a laparotomy (or Mcburnery) was needed. Adhesions were encountered during interval appendectomy; however, conversion was not needed. Median OT was 50 (10–67) minutes with a mean of 40 minutes. Intraoperative complications were limited to 1 case of mild epiploic bleeding related to port insertion managed by bipolar cauterization. No intestinal perforation was encountered. Median postoperative LOS was 2 days. Two patients (5%) had short-term postoperative complications. Both of them had an infra-centimetric umbilical abscess, managed with antiseptic dressings. No long-term complications were noted. No incisional hernias were found, and no intestinal obstruction was diagnosed. Esthetic results were very good, with no evidence of a scar at the month follow of 1 month postoperatively (Fig. 3).

Fig. 3: The aspect of the abdomen at the 1-month postoperative visit
DISCUSSION
Although the gold standard technique for appendectomy is highly debatable,9,10 there is a growing evidence that laparoscopic approach is associated with less postoperative pain, shorter LOS, earlier postoperative recovery, less cutaneous infectious complications, and better cosmetics.7,11 The main drawback of laparoscopic appendectomy was thought to be an increased risk of postoperative intra-abdominal abscess formation, which was reported in initial experiences,9,12 however, large multi-centric studies had shown that this risk probably does not exist.11 Since the introduction of minimal invasive appendectomy,2 and after the increasing understanding of the advantages of minimal invasive approach, surgeons were trying to reduce the number of ports used in the classic 3-port techniques. The appendectomy techniques used today are: the classic 3-port technique, a 2-port technique,13 the single-port laparoscopic appendectomy using either the SILSPort or the glove-port technique,14 and the TULLA.
The advantages of TULLA were numerous. The installation was easy. There was no need to assemble a port; instead a classic 10 mm port was needed. Good patient positioning was an efficient maneuver to help a better exposure. TULAA was fast and easily reproducible. Using a simple classical non-articulated grasper, no particular technical skills were needed. Extracorporeal appendectomy decreased the need for additional potentially “costy” material, like additional ports, endo-loop, and an endo-bag. The most common reason for conversion in our series was retrocecal-subserosal appendix with/without a non-mobile cecum. In cases of generalized peritonitis, we opted directly for a 3-port technique. This attitude was adopted by other authors.6 Our impression was that aspiration without a counter-traction was not sufficient in cases of generalized peritonitis. We could have used a 2-port technique instead of 3, however, that was not in our protocol. Localized peritonitis was not a reason for a conversion. The last advantage is the cosmetics. One month after surgery, the abdomen was scarless. From here, we felt the importance of family education about the small but existent risk of intestinal obstruction later in life. Though our fastest operative time was short (10 minutes) our mean operative time (40 minutes) was longer than other series.6 We think that with further experience in this technique, the operative time might decrease. Regarding the complications, when generalized peritonitis cases were excluded, we don’t think it’s meaningful to compare the incidence of intra-abdominal infections and digestive complications (like intestinal perforation) with the conventional 3-port technique as patient’s population differs. However, wound infection seemed to be the main drawback to this technique.15 In accordance with larger multiple series,7 we had 5% umbilical skin superficial infection. The reason was probably related to the contact of the infected appendix with the abdominal wall, although vigorous incisional cleansing was always done before the closure. The installation of a protector retractor of Alexis-type might be advantageous in those cases, however, this was not proven to decrease the risk of infections.16
CONCLUSION
We had a small population number, so definite conclusions could not be drawn. Despite this, we feel that the main advantages of this technique remain: the scarless, easily reproducible, safe, and low-cost surgery. We think it should be attempted every time a generalized peritonitis is not suspected.
SUPPLEMENTARY MATERIAL
A Supplementary Video to this article is available online on the website of www.wjols.com.
REFERENCES
1. McBurney C. The incision made in the abdominal wall in cases of appendicitis, with a description of a new method of operating. Ann Surg 1894;20(1):38–43. DOI: 10.1097/00000658-189407000-00004.
2. Semm K. Endoscopic appendectomy. Endoscopy 1983;15(2):59–64. DOI: 10.1055/s-2007-1021466.
3. Roberts KE. True single port appendectomy: first experience with the puppeteer technique. Surg Endosc 2009;23(8):1825–1830. DOI: 10.1007/s00464-008-0270-9.
4. Ateş O, Hakgüder G, Olguner M, et al. Single-port laparoscopic appendectomy conducted intracorporeally with the aid of a transabdominal sling suture. J Pediatr Surg 2007;42(6):1071–1074. DOI: 10.1016/j.jpedsurg.2007.01.065.
5. Hernandez-Martin S, Ayuso L, Molina AY, et al. Transumbilical laparoscopic-assisted appendectomy in children: is it worth it? Surg Endosc 2017;31(12):5372–5380. DOI: 10.1007/s00464-017-5618-6.
6. Esparaz JR, Jeziorczak PM, Mowrer AR, et al. Adopting single-incision laparoscopic appendectomy in children: is it safe during the learning curve? J Laparoendosc Adv Surg Tech A 2019;29(10):1306–1310. DOI: 10.1089/lap.2019.0112.
7. Gasior AC, St. Peter SD, Knott EM, et al. National trends in approach and outcomes with appendicitis in children. J Pediatr Surg 2012:2264–2267. DOI: 10.1016/j.jpedsurg.2012.09.019.
8. Schier F. Laparoscopic appendectomy with 1.7-mm instruments. Pediatr Surg Int 1998;14(1–2):142–143. DOI: 10.1007/s003830050465.
9. Park J, Kwak H, Kim SG, et al. Single-port laparoscopic appendectomy: comparison with conventional laparoscopic appendectomy. J Laparoendosc Adv Surg Tech A 2012;22(2):142–145. DOI: 10.1089/lap.2011.0253.
10. Pappalepore N, Tursini S,Marino N, et al. Transumilical laparoscopic-assisted appendectomy (TULLA): a safe and useful alternative for uncomplicated appendicitis. Eur J Pediatr Surg 2002;12(6):383–386. DOI: 10.1055/s-2002-36846.
11. St. Peter SD, Adibe OO, Juang D, et al. Single incision versus standard 3-port laparoscopic appendectomy: a prospective randomized trial. Ann Surg 2011;254(4):586–590. DOI: 10.1097/SLA.0b013e31823003b5.
12. Jin SG, Cho SH, Kim KY, et al. Transumbilical single-incision laparoscopic-assisted appendectomy (TULAA) is useful in adults and young adolescents: comparison with multi-port laparoscopic appendectomy. Medicina 2019;55(6):248. DOI: 10.3390/medicina55060248.
13. Akkary R, Zeidan S, Matta R, et al. Pediatric appendectomy in the developing countries. How does it differ from the international experience? Int J Pediatr Adolesc Med 2019;7(2):70–73. DOI: 10.1016/j.ijpam.2019.06.006.
14. Rentea RM, and St. Peter SD. Pediatric appendicitis. Surg Clin North Am 2017;97(1):93–112. DOI: 10.1016/j.suc.2016.08.009.
15. Shekherdimian S and DeUgarte D. Transumbilical laparoscopic-assisted appendectomy: an extracorporeal single-incision alternative to conventional laparoscopic techniques. Am Surg 2011;77(5):557–560. DOI: 10.1177/000313481107700513.
16. Aziz O, Athanasiou T, Tekkis PP, et al. Laparoscopic versus open appendectomy in children: a meta-analysis. Ann Surg 2006;243(1):17–27. DOI: 10.1097/01.sla.0000193602.74417.14.
________________________
© The Author(s). 2022 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.